Back and Peripheral Joint Disorders due to:
Arthritis, degenerative or inflammatory

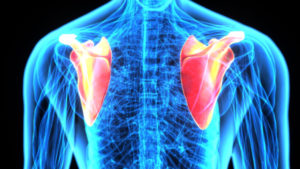
Many people start to feel pain and stiffness in their bodies over time. Sometimes their hands or knees or shoulders get sore and are hard to move and may become swollen. These people may have arthritis. Arthritis may be caused by inflammation of the tissue lining the joints. Some signs of inflammation include redness, heat, pain, and swelling. These problems are telling you that something is wrong.
Joints are places where two bones meet, such as your elbow or knee. Over time, in some types of arthritis but not in all, the joints involved can become severely damaged.
There are different types of arthritis. In some diseases in which arthritis occurs, other organs, such as your eyes, your chest, or your skin, can also be affected. Some people may worry that arthritis means they won’t be able to work or take care of their children and their family. Others think that you just have to accept things like arthritis.
Failed Back Syndrome
Failed back surgery syndrome (also called FBSS, or failed back syndrome) is a misnomer, as it is not actually a syndrome – it is a very generalized term that is often used to describe the condition of patients who have not had a successful result with back surgery or spine surgery and have experienced continued pain after surgery. There is no equivalent term for failed back surgery syndrome in any other type of surgery (e.g. there is no failed cardiac surgery syndrome, failed knee surgery syndrome, etc.).
There are many reasons that a back surgery may or may not work, and even with the best surgeon and for the best indications, spine surgery is no more than 95% predictive of a successful result.
Sciatica
Sciatica is a symptom of a problem with the sciatic nerve, a large nerve that runs from the lower back down the back of each leg. It controls muscles in the back of your knee and lower leg and provides feeling to the back of your thigh, part of your lower leg and the sole of your foot. When you have sciatica, you have pain, weakness, numbness or tingling. It can start in the lower back and extend down your leg to your calf, foot, or even your toes. It’s usually on only one side of your body.
Sciatica may be due to a ruptured intervertebral disk, narrowing of the spinal canal that puts pressure on the nerve called spinal stenosis, or an injury such as a pelvic fracture. In many cases, no cause can be found.
Sometimes sciatica goes away on its own. Treatment, if needed, depends on the cause of the problem. It may include exercises, medicines and surgery.
Scoliosis
 Scoliosis is a problem with the curve in the spine Many people have some curve in their spine. But a few people have spines that make a large curve from side to side in the shape of the letter “S” or the letter “C.” If this curve is severe, it can cause pain and make breathing difficult. The good news is that most cases of scoliosis are mild. If found early, they can usually be prevented from getting worse.
Scoliosis is a problem with the curve in the spine Many people have some curve in their spine. But a few people have spines that make a large curve from side to side in the shape of the letter “S” or the letter “C.” If this curve is severe, it can cause pain and make breathing difficult. The good news is that most cases of scoliosis are mild. If found early, they can usually be prevented from getting worse.
Spinal Stenosis
Spinal stenosis is a narrowing of one or more areas in your spine — most often in your upper (cervical) or lower (lumbar) spine. This narrowing can put pressure on your spinal cord or on the nerves that branch out from the compressed areas. Spinal stenosis can cause pain, numbness, tingling or cramping in your legs, back, neck, shoulders or arms; a loss of sensation in your extremities; and sometimes problems with bladder or bowel function. Spinal stenosis is most commonly caused by osteoarthritis-related bone damage.
Spinal narrowing doesn’t always cause problems, but if the narrowed areas compress the spinal cord or spinal nerves, you’re likely to develop inflammation of nerves that can cause signs and symptoms. These often start gradually and grow worse over time.
Sports Injuries
Sports injuries are common at every age and can often have lasting effects. When your painful sports injury lasts for more than a few weeks, it is important to see a sports injury pain relief treatment specialist to help ensure your pain does not become chronic pain. After a full evaluation, a sports injury pain treatment specialist can tailor a sports injury pain relief plan according to your needs and help you return to the playing field, court, course or even just the backyard. The most common sports injuries are strains and sprains. Sprains are injuries to ligaments, the tough bands connecting bones in a joint. Suddenly stretching ligaments past their limits deforms or tears them. Strains are injuries to muscle fibers or tendons, which anchor muscles to bones. Strains are called “pulled muscles” for a reason: Over-stretching or overusing a muscle causes tears in the muscle fibers or tendons.
Virginia Medical Marijuana Certificates
Currently, patients with symptoms from any condition or disease that our licensed Physician whom is currently registered with the VA Board of Pharmacy, that would benefit from THC-A or CBD qualifies for written certification. Thanks to the provisions outlined in §54.1-3408.3, patients with a debilitating medical condition can now pursue treatment using THC-A or CBD after receiving a written certification from their practitioner to manage the symptoms of their condition. For more information visit norml.org.
Neuropathic pain due to:
Diabetes-related neuropathy
Neuropathy, a common complication of diabetes, is damage to the nerves that allow you to feel sensations such as pain. There are a number of ways that diabetes damages the nerves, and they are all linked to blood glucose (sugar) being too high for a long period of time.
Diabetes-related nerve damage can be painful, but it isn’t severe in most cases. There are two major types of diabetic neuropathy: peripheral and autonomic.
Chronic Pain Related to:
Cancer
Unfortunately, people who develop cancer, often suffer from cancer-related pains. The cancer cells can invade bones, nerves, organs and other structures in the body. The pressure or the destruction of normal tissue can cause severe pain.
There are also patients that may have cancer without cancer-related pain, but have pre-existing or develop painful conditions such as degenerative joint disease, degenerative disc disease, sciatica etc. after a diagnosis of cancer that can be treated to improve function and quality of life.
During our consultations, we obtain a complete medical history and gather as much information as possible on a patient’s pain and it impact on their life. We work with each patient on a one-to-one basis to determine the best treatment plan for their individual pain, utilizing the most advanced techniques to improve symptoms and allow for increased participation in everyday activities.
Treatments for patients with cancer focus on relieving symptoms and can vary depending on the cause and severity of a patient’s individual condition, as well as their overall health and medical history. The most successful pain management programs are those that are specifically tailored to a patient’s needs, enabling them to maximize their independence and capability.
Complex Regional Pain Syndrome (CRPS/RSD)
Complex regional pain syndrome (CRPS), formerly known as Regional Sympathetic Dystrophy (RSD), is an uncommon, chronic condition that affects the nervous system that usually affects your extremities. The cause of CRPS isn’t clearly understood, though it often follows an illness or injury.
CRPS usually presents as an intense burning or aching pain. Patients with CRPS may also experience swelling, skin discoloration, altered temperature, abnormal sweating, hypersensitivity, changes in hair & nail growth patterns, muscle spasms, weakness and decreased ability to move the affected body part.
Symptoms may change over time and vary from person to person. Once these changes occur, the condition is often irreversible. This is why it is important to treat complex regional pain syndrome. In such cases, dramatic improvements may be possible.
Fibromyalgia
Fibromyalgia is a poorly understood complex, chronic disorder. It can cause widespread pain and stiffness, poor sleep and fatigue. It is often associated with other conditions including depression, anxiety, headaches, swelling of extremities, irritable bowel syndrome, and restless leg syndrome among others. It typically was a waxing & waning pattern that can be affected by weather changes, stress, overexertion, illness or surgery. The goal of treatment is to reduce symptoms and improve function, as there is no known cure. While treatment regimens vary widely, physical activity is of utmost importance.
Headaches/Migraines
 A headache is a common symptom that involves pain in one or more areas of the head or face. Over 45 million people are affected by headaches each year and many of them include chronic headaches that last for weeks or months with no relief.
A headache is a common symptom that involves pain in one or more areas of the head or face. Over 45 million people are affected by headaches each year and many of them include chronic headaches that last for weeks or months with no relief.
Migraine headaches can cause intense throbbing or a pulsing sensation in one area of the head and are commonly accompanied by nausea, vomiting and extreme sensitivity to light and sound. Migraine attacks can cause significant pain for hours to days. Some migraines are preceded or accompanied by sensory warning symptoms known as an aura, such as flashes of light, blind spots, or tingling.
Cluster headaches are a type of headache that has a characteristic grouping of attacks. Cluster headaches occur up to 8 times per day during a cluster period, which may last 2 weeks to 3 months or longer. The headaches may disappear completely (go into remission) for months or years, only to recur at a later date. A cluster headache typically wakes a person from sleep 1 to 2 hours after going to bed. A cluster headache has no structural cause, and the biochemical cause is unknown. However, the headaches occur with the trigeminal nerve pattern. They are typically on one side of the face, behind an eye that may radiate to other parts of the face usually described as a piercing or ice pick type of pain.
Tension headaches are generally a diffuse mild to moderate pain in the head that is often described as a tight band around the head. A tension headache is the most common type of headache, yet its causes are not well understood. The most common theories support a heightened sensitivity to pain and possibly heightened sensitivity to stress. Stress is the most commonly reported trigger for tension headaches.
Post-Operative Pain
 The effective relief of pain is of the utmost importance to anyone treating patients who have recently had surgery. Pain relief has significant physiological benefits; hence, monitoring of pain relief is increasingly becoming an important postoperative quality measure. The goal for postoperative pain management is to reduce or eliminate pain and discomfort with a minimum of side effects. Various agents (opioid vs. nonopioid), routes (oral, intravenous, neuraxial, regional) and modes (patient controlled vs. “as needed”) for the treatment of postoperative pain exist. Although traditionally the mainstay of postoperative analgesia is opioid-based, increasingly more evidence exists to support a multimodal approach with the intent to reduce opioid side effects (such as nausea and ileus) and improve pain scores.
The effective relief of pain is of the utmost importance to anyone treating patients who have recently had surgery. Pain relief has significant physiological benefits; hence, monitoring of pain relief is increasingly becoming an important postoperative quality measure. The goal for postoperative pain management is to reduce or eliminate pain and discomfort with a minimum of side effects. Various agents (opioid vs. nonopioid), routes (oral, intravenous, neuraxial, regional) and modes (patient controlled vs. “as needed”) for the treatment of postoperative pain exist. Although traditionally the mainstay of postoperative analgesia is opioid-based, increasingly more evidence exists to support a multimodal approach with the intent to reduce opioid side effects (such as nausea and ileus) and improve pain scores.
Each patient is unique in his or her perception of pain allowing for many combinations in the treatment of pain. The introduction of enhanced recovery programs for colorectal surgery have changed both physician and patient expectations in terms of perioperative pain management making the reduction of opiate intake a factor in meeting these expectations. In conclusion, multimodal pain management therapy should be used whenever possible.